DIABETIC RETINOPATHY
Diabetes is one of the the leading causes of vision loss in the world. In the United States, it is the most common cause of vision loss in young people. People with diabetes may have mild diabetic eye disease for many years. We know that high blood sugar and other metabolic abnormalities in diabetics can damage blood vessels in the body. When these blood vessels are damaged, blood flow to parts of the body is affected resulting in damage to the organs. Some of the tissues that are most sensitive to reduced blood flow and oxygen supply include the feet, heart, kidneys, and the eyes. Retina is one of the most vitals parts of the eye affected by diabetes. Damage to retinal blood vessels can cause bleeding, swelling of the retina, insufficient blood flow to the retina, and scarring of the retina.
In the long run, people with diabetes who have better blood sugar control will have fewer problems. The most important way to prevent eye diseases related to diabetes is to maintain strict blood sugar control. High blood pressure and high levels of lipids or cholesterol should also be treated because these diseases can exacerbate retinal diseases caused by diabetes. In mild cases of diabetic eye disease, vision can remain stable for many years. In many cases, depending on severity and type of diabetes related damage to the retina, laser, intraocular injections, and eye surgery may be recommended to improve vision. There are two main stages of diabetic retinopathy. The first stage of diabetic retinopathy is called non-proliferative diabetic retinopathy. The more advanced stage of diabetic retinopathy is called proliferative diabetic retinopathy.
Non-proliferative Diabetic Retinopathy
High blood sugar levels can damage the walls of small blood vessels in the retina over a period of time. These small blood vessels can begin to have cumulative damage over time. Due to this, fluid (edema), protein deposits (hard exudate), and blood (bleeding) accumulate in the retina. Affected blood vessels also develop “wall pouching” called microaneurysm, one of the first signs of diabetic eye disease. This process of retinal damage and blood leakage is called Non-proliferative diabetic retinopathy. If fluid builds up in the center of the retina (called the macula), it leads to a condition called diabetic macular edema. In severe cases of blood vessel damage, the tiny capillaries that provide the center of vision (the macula) can be closed permanently causing a condition called macular ischemia.
Treatments: Non-proliferative Diabetic Retinopathy

Laser therapy
Non-proliferative diabetic retinopathy related macular edema can be treated with laser. This therapy is done in the office and the laser focuses a light beam to treat leaky blood vessels in the area of the macula. This has been shown to reduce the risk of vision loss due to macular edema.
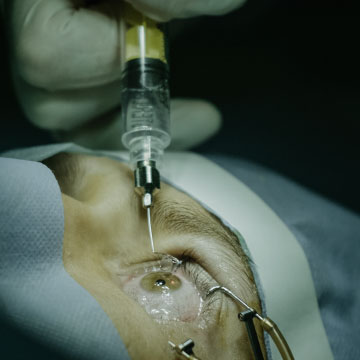
Intraocular Injection
One of the most common treatments for treatment of macular edema in diabetic retinopathy patients is with intraocular injection. These include treatment with different medications such as anti-inflammatory steroid injections, Avastin®, Eylea®, and Lucentis®. The procedure is done very quickly and painlessly in the clinic.

Vitrectomy
In some cases, the vitreous gel and the membrane on the surface of the retina may be contributing to macular edema. In these cases, vitrectomy surgery may help with edema. With the help of fine instruments retina specialist can remove the membranes which can result in improvement in vision.
Treatments: Non-proliferative Diabetic Retinopathy
Damage to blood vessels caused by high blood sugar levels eventually reduces blood flow and reduces oxygen delivered to the retina. In response to a compromised supply of oxygen to the retina, the body can create new blood vessels that grow on the surface of the retina. The process by which new blood vessels are formed is called retinal neovascularization. This is a hallmark of proliferative diabetic retinopathy. These new vessels are actually more harmful than beneficial. The new blood vessels are very weak and unstable. If left untreated, they can cause bleeding and scar tissue to form inside the eye. The scar tissue can contract and stretch the retina, causing the retina to detach from underlying layers. This often causes severe vision loss. In an advanced stage of the disease, this vision loss can be permanent. Early detection and treatment are imperative to prevent vision loss due to proliferative diabetic retinopathy. In severe cases, neovascularization of the iris may develop in the front of the eye (the colored part of the eye). If abnormal vessels develop in the iris, they can block the drainage angle of the the eye and cause a very steep increase in pressure inside the eye. This condition is called a neovascular glaucoma and can cause severe eye pain and loss of vision.
Treatment: Proliferative Diabetic Retinopathy
Proliferative diabetic retinopathy is treated with a combination of intraocular injections and laser treatment in the clinic. Sometimes surgical treatment is required in the operating room.

Laser Therapy (PRP):
Pan-retinal photocoagulation (PRP) is a laser procedure that suppresses production of neovascularization. This procedure is usually performed in a doctor’s office under local anesthesia. Pan-retinal photocoagulation has been shown to reduce the risk of vision loss due to proliferative diabetic retinopathy.

Vitrectomy:
If a large number of new blood vessels develop and cause scarring or bleeding in the eye then a vitrectomy procedure is sometimes indicated. This operation is performed in a surgery center or hospital operating room. During the procedure blood is removed from the eye and replaced with clear fluid. A scar can be removed from the surface of the retina with sensitive instruments.
